On the deck of a sportfishing boat on a sparkling Saturday morning in Mexico’s Gulf of California, Raymond Schinazi is singing.
Sky of blue
Sea of green
In my yellow submarine
The fish aren’t biting, but this 65-year-old organic chemist from Emory University in Atlanta is delighted to watch the humpback whales spout, soak up the Baja sun, and be out of cell tower range. “There is lots of sea, and there are lots of fish,” he says after a few hours pass without landing a big one. “You have to be an optimist.”
The name of the boat is No Big Deal.
Few scientists who work in academia have benefited more from big deals than Schinazi. He specializes in the synthesis of so-called nucleoside and nucleotide drugs that interfere with viral replication—an idea once widely dismissed. Two years ago, Schinazi pocketed $440 million on a deal involving sofosbuvir, a yellow submarine–shaped pill that has revolutionized hepatitis C (HCV) treatment and had blockbuster sales for Gilead Sciences of Foster City, California. In 2005, an anti-HIV drug he helped develop, FTC, netted $540 million for Emory—which gave $71 million to Schinazi. Emory and Schinazi have made millions more in royalty fees for a sister drug, 3TC, which treats both HIV and hepatitis B. And Schinazi, who also runs a lab at Atlanta’s VA Medical Center, had a hand in two other drugs on the market. He holds more than 90 patents and recently helped form a company that he contends will make still more effective drugs against hepatitis B and C. But on his way up, Schinazi has rocked a few boats.
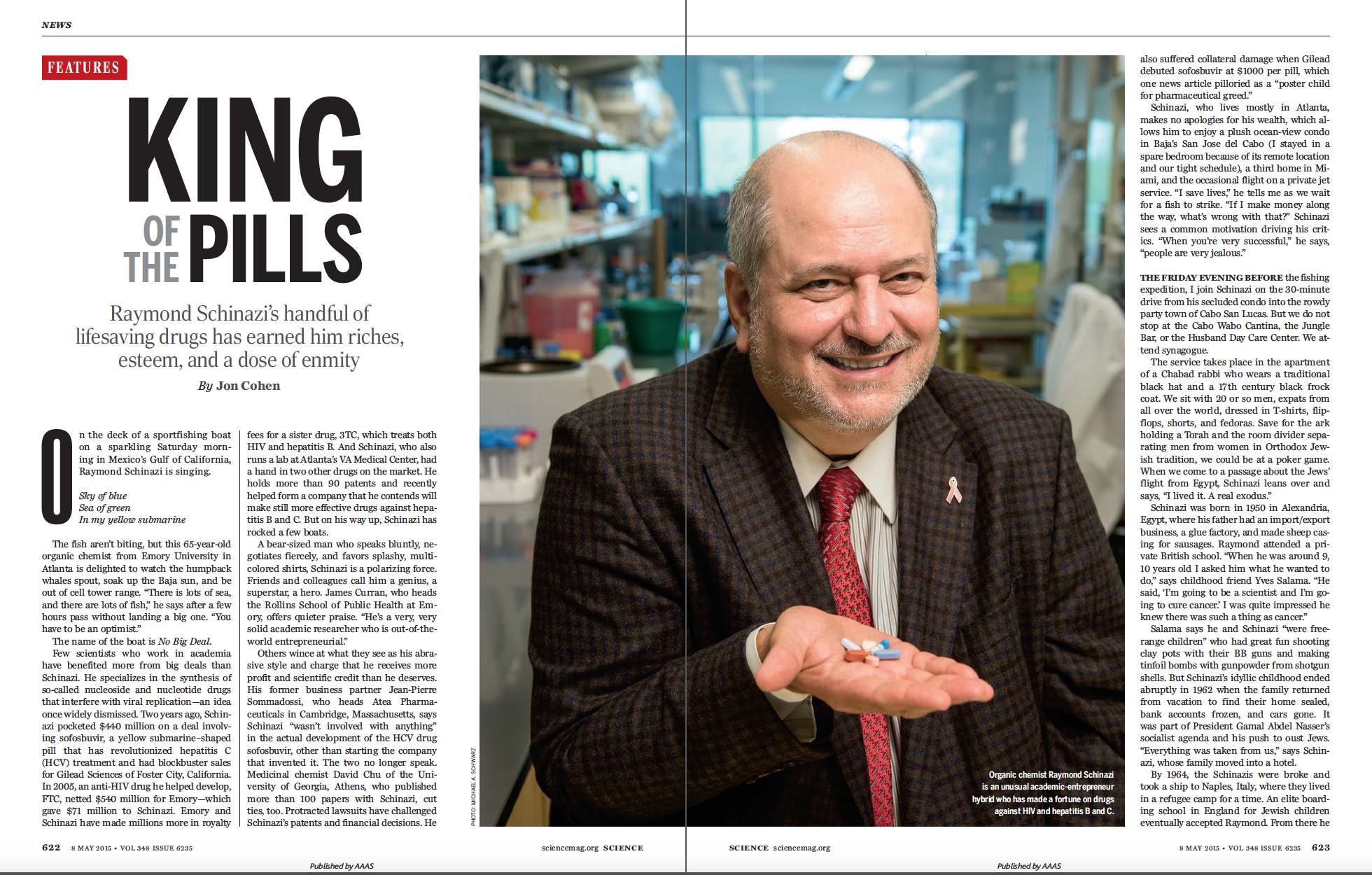
A bear-sized man who speaks bluntly, negotiates fiercely, and favors splashy, multicolored shirts, Schinazi is a polarizing force. Friends and colleagues call him a genius, a superstar, a hero. James Curran, who heads the Rollins School of Public Health at Emory, offers quieter praise. “He’s a very, very solid academic researcher who is out-of-the-world entrepreneurial.”
Others wince at what they see as his abrasive style and charge that he receives more profit and scientific credit than he deserves. His former business partner Jean-Pierre Sommadossi, who heads Atea Pharmaceuticals in Cambridge, Massachusetts, says Schinazi “wasn’t involved with anything” in the actual development of the HCV drug sofosbuvir, other than starting the company that invented it. The two no longer speak. Medicinal chemist David Chu of the University of Georgia, Athens, who published more than 100 papers with Schinazi, cut ties, too. Protracted lawsuits have challenged Schinazi’s patents and financial decisions. He also suffered collateral damage when Gilead debuted sofosbuvir at $1000 per pill, which one news article pilloried as a “poster child for pharmaceutical greed.”
PHOTO: MICHAEL A. SCHWARZ
Schinazi, who lives mostly in Atlanta, makes no apologies for his wealth, which allows him to enjoy a plush ocean-view condo in Baja’s San Jose del Cabo (I stayed in a spare bedroom because of its remote location and our tight schedule), a third home in Miami, and the occasional flight on a private jet service. “I save lives,” he tells me as we wait for a fish to strike. “If I make money along the way, what’s wrong with that?” Schinazi sees a common motivation driving his critics. “When you’re very successful,” he says, “people are very jealous.”
THE FRIDAY EVENING BEFORE the fishing expedition, I join Schinazi on the 30-minute drive from his secluded condo into the rowdy party town of Cabo San Lucas. But we do not stop at the Cabo Wabo Cantina, the Jungle Bar, or the Husband Day Care Center. We attend synagogue.
The service takes place in the apartment of a Chabad rabbi who wears a traditional black hat and a 17th century black frock coat. We sit with 20 or so men, expats from all over the world, dressed in T-shirts, flipflops, shorts, and fedoras. Save for the ark holding a Torah and the room divider separating men from women in Orthodox Jewish tradition, we could be at a poker game. When we come to a passage about the Jews’ flight from Egypt, Schinazi leans over and says, “I lived it. A real exodus.”
Schinazi was born in 1950 in Alexandria, Egypt, where his father had an import/export business, a glue factory, and made sheep casing for sausages. Raymond attended a private British school. “When he was around 9, 10 years old I asked him what he wanted to do,” says childhood friend Yves Salama. “He said, ‘I’m going to be a scientist and I’m going to cure cancer.’ I was quite impressed he knew there was such a thing as cancer.”
Salama says he and Schinazi “were free-range children” who had great fun shooting clay pots with their BB guns and making tinfoil bombs with gunpowder from shotgun shells. But Schinazi’s idyllic childhood ended abruptly in 1962 when the family returned from vacation to find their home sealed, bank accounts frozen, and cars gone. It was part of President Gamal Abdel Nasser’s socialist agenda and his push to oust Jews. “Everything was taken from us,” says Schinazi, whose family moved into a hotel.
By 1964, the Schinazis were broke and took a ship to Naples, Italy, where they lived in a refugee camp for a time. An elite boarding school in England for Jewish children eventually accepted Raymond. From there he went to England’s University of Bath, where he completed an undergraduate degree and a Ph.D. in chemistry. He lived on 100 English pounds a month, working as a parking attendant to help pay his way, and didn’t have real money in his pocket until he won 3000 pounds in the Spanish lottery.
While at Bath, Schinazi met his mother’s brother, pediatrician André Nahmias, who left Egypt before his nephew was born and had become a well-known herpesvirus researcher at Emory. Nahmias helped Schinazi secure a postdoc at Yale with William Prusoff, a chemist dubbed “the father of antiviral chemotherapy.” Prusoff synthesized the first antiviral used in clinical practice, a drug called idoxuridine that treats herpes infection of the eye. It is a synthetic nucleoside.
Nucleosides are chemical precursors to the nucleotides that make up DNA and RNA. When viruses copy themselves, they string together nucleotides. Chemical modifications can create defective analogs of these building blocks. Viruses incorporate them into a growing chain of nucleotides but usually cannot add new links, gumming up production of genetic material and aborting viral replication.
Nucleotide analogs typically make lousy drugs: The molecules are highly charged and have difficulty entering cells. Not so for nucleoside analogs, which cells convert into nucleotides. But they can cause serious toxicities if they get into human DNA or RNA. At the time Schinazi joined Prusoff’s lab in 1976, many drug developers shunned them.
After 3 years with Prusoff making nucleoside analogs, Schinazi moved to Emory to study viruses and immunology with his uncle. “I knew that the glory was in biology,” he says. “I wanted to save the world.” But he was confident that his aptitude for chemistry would help. “I look at structures and they mean something to me,” he says. “It’s a language.”
BRENDAN LARDER MET SCHINAZI in the early 1980s when he exited a herpesvirus conference held at the University of Oxford and stepped into the street. “A car pulled up on the sidewalk, a window came down, and a voice said, ‘Get in,’” recalls Larder, who was then working on his Ph.D. in virology. Schinazi knew that Larder was studying acyclovir, a nucleoside analog being developed by Burroughs Wellcome to treat herpesvirus, and wanted to pick his brain. In those days, Larder says, Schinazi “was not at all prominent.”
Larder tells me this story at a swank hotel in Key Biscayne, Florida, where 125 researchers gathered in December 2014 for HIV DART, a biennial conference on HIV drug development that Schinazi co-organizes. (He hosts a similar hepatitis meeting in Hawaii.) Many of the attendees wear the colorful meeting T-shirt, sporting an aerial view of Miami that Schinazi shot from his nearby condo. “If you ask a lot of people why did you come here, they’ll say, ‘Because Ray asked me to,’” says Larder, who for years worked at Wellcome and now heads the HIV Resistance Response Database Initiative, a nonprofit based in London. “It’s a way to bring his friends together. Ray does polarize opinions and people’s emotions, but more people love him than hate him.”
One morning, Schinazi gives the David Barry DART Achievement Award. He sings the praises of the deceased Barry, who once directed research at Wellcome and helped develop AZT, the first anti-HIV drug. He makes no mention of their complicated history. “David Barry was my arch enemy,” Schinazi tells me during a meeting break.
In 1986, Schinazi—independent of Wellcome—synthesized AZT and gave it to Sommadossi, a pharmacologist then with the University of Alabama, Birmingham. Sommadossi proceeded to show that it had toxic effects on bone marrow cells. Barry, anxious about AZT’s imminent approval by the U.S. Food and Drug Administration (FDA), dismissed the results, Schinazi says, asserting that they were due to impurities in the compound he had made. “He was a big shot and I was a nothing,” Schinazi says. “He hated me.” The toxicity soon surfaced in human studies, but the FDA approved the drug nonetheless in March 1987. That same year, Schinazi helped Prusoff’s lab show that another nucleoside analog, d4T, had activity against HIV—and it later would come to market. But it was a third AIDS drug dubbed 3TC that elevated Schinazi to the big leagues.
In 1989, he learned of a potential drug developed by a Canadian biotech, BioChem International. The drug, a synthetic nucleoside, contained an equal mixture of mirror-image “enantiomers”—left- and right-hand versions of the same molecule. Because enantiomers can have different powers and toxicities, Schinazi saw an opportunity. He enlisted Dennis Liotta, a chemist at Emory, to see if they could sort out the enantiomers. “I was a pretty good chemist and Ray had a background in virology,” Liotta says. “It turned out to be an excellent combination.”
With help from one of Liotta’s postdocs, the team found a chemical reaction that efficiently separated the enantiomers. The left-handed enantiomer, 3TC, was more potent, and they then synthesized a closely related compound, FTC, that included a fluorine atom. Subsequent studies showed that the drugs also had activity against hepatitis B virus. Schinazi had to lobby Emory to file patents for their compounds. “He’s got natural entrepreneurial talents that most people have to teach themselves,” Liotta says. “I think he can smell money.”
IN 1993, LARDER LED a Wellcome team that found a remarkable test-tube effect of 3TC and FTC: HIVs that mutated and became resistant to these drugs became more sensitive to AZT. The synergy meant lower, far less toxic doses of AZT, plus it gave 3TC and FTC a new reason for being. Novel combination therapies were in the offing.
The next year, pharmaceutical giant Glaxo merged with Wellcome, leading Barry and a host of his colleagues to defect and form Triangle Pharmaceuticals. They joined forces with Schinazi, Liotta, and Chu, who had potential drugs on their university shelves. “[Barry] probably teamed up with Ray because his enemy became Glaxo,” Larder says.
The unusual synergistic features of 3TC and FTC—and their obvious market potentials —led to a tangle of lawsuits, with Emory suing Glaxo and BioChem for patent infringement on 3TC, countersuits, and similar fights over FTC. The cases were all settled, transforming the fortunes of Schinazi and Liotta—and Emory.
Triangle’s slow progress frustrated Schinazi, so he and Sommadossi formed two new drug companies in 1998 to focus on nucleoside analogs. “They weren’t taking any of our compounds, and I could see my technology sitting on a shelf,” Schinazi says. “I like speed.” Schinazi headed one, Pharmasset, while Sommadossi ran the other, Idenix. “Both companies made some great scientific discoveries when nucleosides were basically considered poor science,” Sommadossi says.
Schinazi had a heart attack in 1998 while attending a meeting at Triangle. “Too much stress,” he says. “More than 30 years no vacation, in the trenches, writing grants, trying to survive. I work too hard. You can ask my ex-wife.” Barry drove him to the hospital, where they discovered that Schinazi, then 48, had an arterial blockage known as a widowmaker. “You try to form two companies simultaneously,” he says. “It almost killed me.”
Adding to his workload, Schinazi, Sommadossi, and a few other aggrieved researchers launched HIV DART that year because the main annual HIV/AIDS meeting in North America—the Conference on Retroviruses and Opportunistic Infections (CROI)—had repeatedly rejected many of their submissions. “We told the CROI people, ‘Next time, if you don’t accept our abstracts, we’re going to move our meeting to exactly the same date as CROI,’” Schinazi says. HIV DART made its debut in December 1998, in St. Thomas, the U.S. Virgin Islands, while CROI took place in the harsh winter of Chicago. “I know how to play hardball,” Schinazi says.
CROI has never invited Schinazi to give an honorary presentation or a plenary talk. He feigns indifference, but he also says the organizers are missing an opportunity to open attendees’ eyes to the drug discovery process. He says it is a lot like fishing. During our expedition, I try to reel in the only big fish we hit that day, but I clumsily snap the line at the last moment. Schinazi consoles me by explaining that this is the story of his life. “Drug discovery, you have to hook it and reel it in—and many things happen along the way,” he says. “You don’t know what you have until the end of the story. You can lose it at any time.”
TODAY, POPULAR ANTI-HIV drugs that have the brand names Combivir, Trizivir, Truvada, and Atripla all contain either 3TC or FTC. Add in d4T (its use is being phased out), and Emory estimates that some 94% of the people infected by HIV who have received treatment have taken one of the drugs Schinazi helped develop (see 648).
These drugs made Schinazi rich, but the hepatitis drug sofosbuvir made him super rich. Sofosbuvir, a nucleotide analog (it masks the negative charge), must be taken in combination with another drug, but unlike older HCV treatments, it has no serious side effects, works against virtually all variations of the virus, and reduces the time to a cure from 48 to 12 weeks. Gilead bought Pharmasset for $11.4 billion to obtain sofosbuvir, which racked up more than $10 billion in sales last year, second only to one other drug on the market. But in the yin-yang of Schinazi’s life, this great success has brought him greater scrutiny than ever.
First and foremost is sofosbuvir’s price tag of $1000 per pill. Gilead set the price, he notes, which he calls “obscene.” But at the same time, he blasts critics who suggest sofosbuvir’s price is not “reasonable” or “rational”—and that he profited too much. “Is it fair to pay $3 for a bottle of water?” he asks. “Do you complain when you’re thirsty? This is something that cures you from a disease.” And he notes that Gilead has already dropped the price because it now combines the drug with a new HCV drug it makes and sells for $1125 per pill. The company also offers a steep discount for poor countries and allows generic sales; indeed, according to Schinazi—“Look at the irony!”—he helped negotiate a price of about $11 per pill for his home country Egypt, which has the highest prevalence of HCV in the world.
Schinazi’s precise role in sofosbuvir’s discovery is also contentious. He’s the co-author of a 2005 paper that discovered a precursor to the drug. But little of that potential drug reached the liver, where HCV resides. Pharmasset then developed a “prodrug,” sofosbuvir, that becomes active in the liver. “I give credit to Ray: He had the vision to start the company,” says Michael Sofia, one of Pharmasset’s key inventors of the prodrug. But when it comes to sofosbuvir’s discovery, he asserts, forget about Schinazi. “Go to the patents, go to publications—there are over 40 in that space,” Sofia says. “His name’s not there.”
Schinazi claims he now has a spectacular HCV drug in the works. “We should be able to cure hepatitis C with just one drug,” he asserts. In November 2014, he merged his company RFS Pharma with Cocrystal Pharma, which he says also has strong leads on a hepatitis B cure and influenza drugs that work against all strains of the virus. He predicts Cocrystal will be as profitable as Pharmasset—and promises to give away his profits. “Everything I do now I’m giving to my charity,” says Schinazi, who has bankrolled land for a new synagogue in Cabo San Lucas, an exchange program with the University of Bath, and endowed chairs at Emory.
Barbara Stoll, who heads his department at Emory, is astonished that he has not let up. “He could be on a yacht doing nothing, but he is driven to make a contribution,” Stoll says. “Money is nothing at this point.”
Well, not nothing. Since the merger, he boasts to me, Cocrystal Pharma’s stock price has doubled. “Thank you, Raymond Schinazi,” Schinazi says. “Somebody likes my drugs. I’ve got a good reputation.”
One day, I have the temerity to suggest that he has also had a great deal of luck. “Don’t tell me about luck, because I worked very hard,” he all but barks. “Nothing came easy for me. I mean, how many times do I have to be lucky?”
During our 9-hour fishing expedition, luck is definitely not with us. But shortly before we return to dock, one of the rods starts to bend and give out line. A deck hand says it is probably a small tuna. I suggest Schinazi reel it in, but he has no interest. “You take it,” he says. “I only want the big ones.”