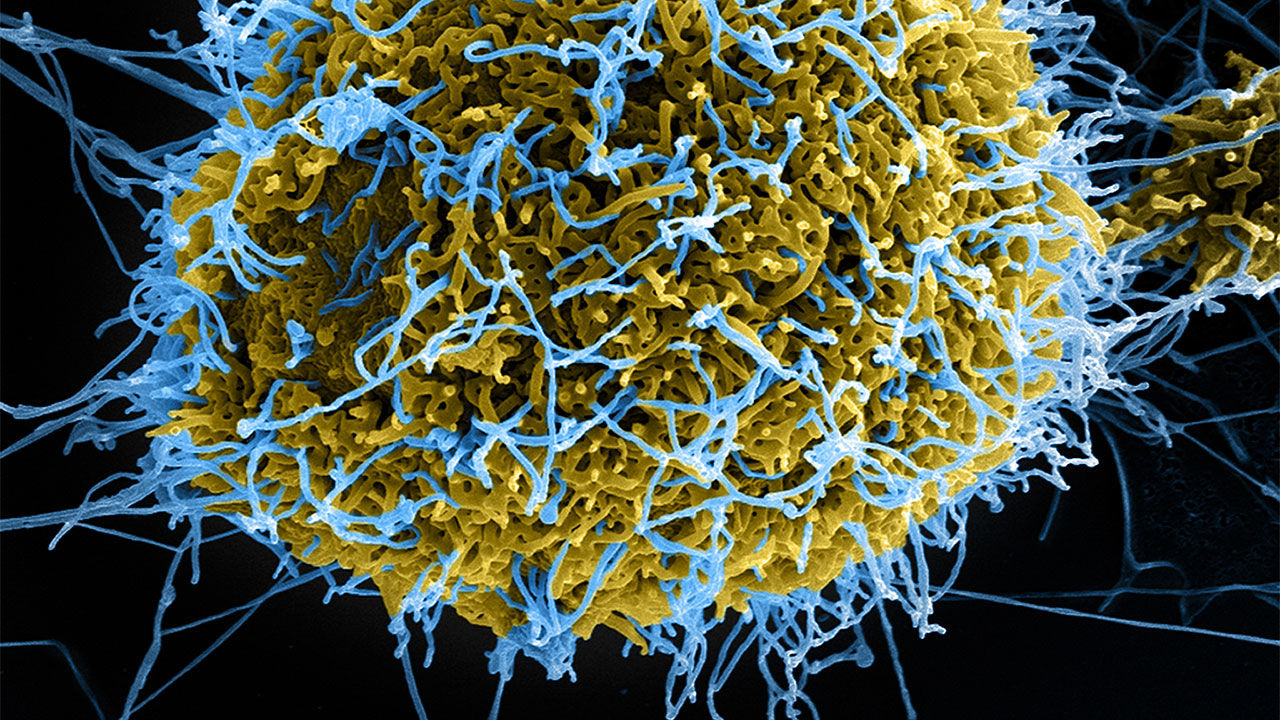
The sheer size of the Ebola epidemic that began in 2013 and engulfed West Africa is still a bit of a riddle for scientists. Previous Ebola outbreaks had never sickened more than 600 people. But the outbreak in Liberia, Sierra Leone, and Guinea infected more than 28,000 before it was finally brought under control. Part of the explanation was that the virus had suddenly surfaced in major cities, making it harder to stamp out than in the isolated rural locales where it had struck before. The countries’ poor public health infrastructure and other environmental factors played roles as well.
But two papers raise another intriguing possibility. They show that some 3 months after the outbreak took off and became a full-blown epidemic, the virus underwent a mutation that made it better suited for humans than for its presumed natural host, a fruit bat species. “The virus has never had this many human-to-human transmissions before, and there are a lot of mutations happening,” says Harvard University’s Pardis Sabeti, an evolutionary geneticist who co-authored one of the papers.
Sabeti stresses that her team only has a “circumstantial” case about the timing of the mutation and the epidemic’s explosion, but her group and an independent team that published the second study have amassed what she calls “compelling evidence” that for the first time links a mutation in the virus to a preference for human cells. The findings “raise the possibility that this mutation contributed directly to greater transmission and thus to the severity of the outbreak,” the team writes. And they found an “association” with increased mortality. “We should neither be alarmist nor complacent,” Sabeti says. “Any possibility that one of the mutations can have a serious impact should be interrogated.”
Working with a team led by Jeremy Luban from the University of Massachusetts Medical School in Worcester, Sabeti and co-workers sequenced samples from 1489 West African patients and analyzed them. By March 2014—about the time the epidemic was detected, but some 3 months after the first case actually occurred—the sequences had split into two distinct lineages, one of which was characterized by a single amino acid change in a region of the virus’s surface protein and allows it to bind to cells. The mutant, Luban says, “completely supplanted the ancestral virus.”
The big question, of course, is whether the mutation could help the virus spread. The researchers did not have access to a biosafety level (BSL) 4 laboratory necessary to test that with the real Ebola virus, so they engineered harmless “pseudotyped” viruses that contained the gene for the surface protein in both its ancestral and mutated form. The mutant far more easily infected human immune cells than did the ancestral pseudotype, the team reports today in Cell. The researchers also showed that the mutant more easily infects primate cells than cells from rodents or carnivores.
The second paper, published today in Cell by a team led by Jonathan Ball at the United Kingdom’s University of Nottingham and Etienne Simon-Loriere of the Pasteur Institute in Paris, independently arrived at a similar conclusion. The team analyzed its own 1610 sequences from the epidemic and also found that they separated into two lineages based on the single mutation in the glycoprotein. The researchers also compared pseudotyped Ebola viruses that matched the ancestor with ones with the same mutation, and found they preferentially infected cells from humans as opposed to the fruit bat species Hypsignathus monstrosus. They also found this mutant’s infectivity was increased by other mutations, which suggests that the virus didn’t undergo just one, but several adaptations allowing it to jump more easily from human to human. That could have complicated attempts to bring the epidemic to an end.
But Ball, Simon-Loriere, and colleagues approach this conclusion most cautiously, stressing that epidemiologic factors, such as “increased circulation in urban areas that in turn led to larger chains of transmission,” likely were the most important driver. “Despite the experimental data provided here, it is impossible to clearly establish whether the adaptive mutations observed were in part responsible for the extended duration of the 2013–16 epidemic,” they write in their paper.
A study published by Science in March of last year did not find any evidence that the virus evolved to become more transmissible or more virulent. But the first author of that paper, virologist Thomas Hoenen of the Friedrich Loeffler Institute in Riems, Germany, says the two new papers make a powerful case that the glycoprotein mutation benefited the virus. “The question now is, what does this really mean in terms of biological consequences?”
Luban stresses that Hoenen’s analysis and others that reached similar conclusions weren’t wrong. But the researchers were analyzing viral sequences to address different questions—such as the viral mutation rate—or only looked at samples isolated in the early days of the outbreak. “You have to do wet experiments sometimes,” Luban says. “All of the algorithm crunching suggested Ebola is Ebola is Ebola. These two experiments say it doesn’t matter what the computers say. The virus is more infectious.”
The authors of the new studies agree that to clarify the impact the mutation has on transmissibility and virulence, scientists must do experiments with the real virus and engineered mutants of it, both in cell cultures and animals. But they have had difficulty finding a BSL-4 lab that’s willing to collaborate and funding is a challenge, too. “We need to pay attention to this,” Sabeti says. The rapid adaptation to humans underscores the need to respond quickly to animal to human transmissions of Ebola and other viruses, she adds. “Anytime you see one of these sparks ignite it could turn into full on forest fire.”